Frequently asked questions
A Client Services team member is also available to help at any time between 8 AM and 8 PM Eastern Time, Monday-Friday.
Email: client.services@foundationmedicine.com
Phone: +1 (888) 988-3639

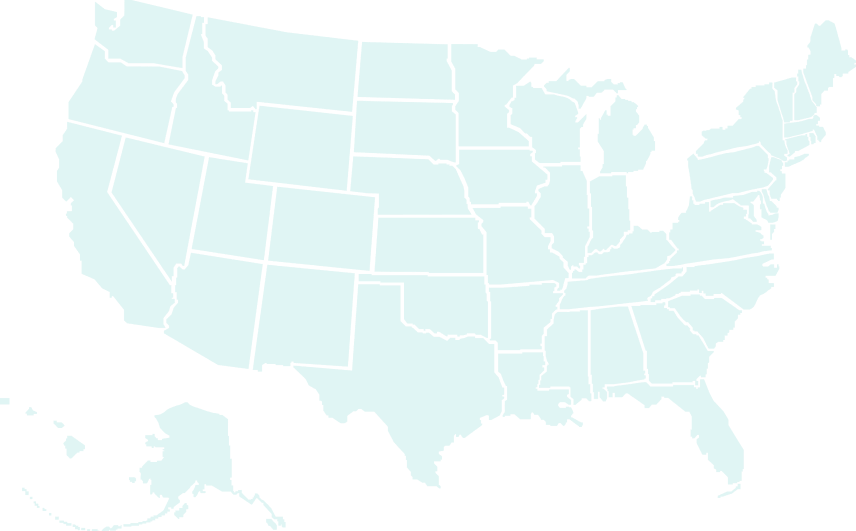
Broad coverage makes our tests more accessible to a greater number of patients.
Search Your State's Coverage →1000+ peer-reviewed publications and 50+ FDA-approved CDx indications make covering our full portfolio an easy decision.
View Evidence Portfolio at this Link →
Foundation Medicine's coverage is continually changing and expanding. Patients should reach
out to their individual health plans to verify their benefits and qualifying medical criteria, as
those details are not represented on this diagram.
Patients who have out-of-pocket costs associated with testing and a financial need may apply for assistance by
completing the online form at aid.foundationmedicine.com. Patients may apply
at any time, even before testing. If approved, qualifying patients will only pay up to $100 for
each test. Financial assistance decisions will be shared with patients within days after their
application is received.

Foundation Medicine has 1000+ peer-reviewed publications. We also have 50+ FDA-approved CDx indications >60% of all approved US companion diagnostic (CDx) indications for NGS testing.
Our tests match specific biomarkers to clinical trials and FDA-approved therapies
Tests with proven accuracy and reliability receive FDA approvals and companion diagnostic indications
Medical necessity gives payers the confidence to cover our full portfolio of tests
Foundation Medicine believes every person with advanced cancer can benefit from precision medicine—and that CGP testing should be accessible to all. Learn how we're making that happen.



When CGP testing is more accessible, biomarker-matched therapies and clinical trials are too—a potentially life-changing opportunity for people with advanced cancer. And with coverage by 20+ state Medicaid plans, we're helping vulnerable patients access the care they need.
paid by qualifying state Medicaid patients
patients owe $0 for testing*
out-of-pocket maximum per test for patients who qualify for financial assistance
We want to make accessing a Foundation Medicine test as easy as possible for you and your patients. Tell us how we can help.